Emergency Dentistry
7 Tooth-Saving Moments Endodontics Was Made For
Sometimes a tooth problem announces itself politely, like a mild zing when you sip something cold. Other times it kicks your plans in the teeth at 2 a.m. with a throbbing pulse that makes you wonder if your jaw has its own heartbeat.
That is the moment endodontics steps in.
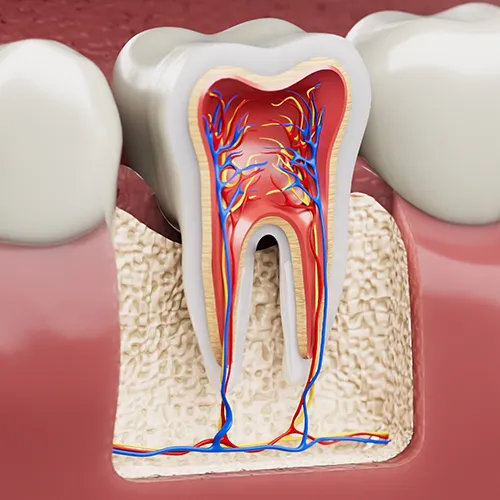
Endodontics is the branch of dentistry focused on the inside of the tooth, specifically the pulp (the soft tissue with nerves and blood vessels) and the roots. The whole goal is simple: get you out of pain, clear the infection or inflammation, and keep your natural tooth whenever possible.
At Akemi Dental Specialists, endodontic care is about being calm, precise, and effective, especially when things feel urgent. If you have been dealing with lingering sensitivity, swelling, pressure, or a tooth that just “doesn’t feel right,” this is for you.
What endodontics actually does (in real-life terms)
Think of your tooth like a house.
- Enamel is the roof and walls.
- Dentin is the framework underneath.
- Pulp is the wiring and plumbing inside.
When the “inside” gets irritated or infected, the outside can still look fine at first. That is why a tooth can hurt badly even when it looks normal in the mirror.
Endodontic treatment is designed to:
- Remove infected or inflamed tissue from inside the tooth.
- Disinfect the root canal system thoroughly.
- Seal the tooth so bacteria cannot keep re-entering.
- Preserve your bite, your smile, and your natural chewing strength.
And yes, root canal treatment is the best-known endodontic procedure, but endodontics also includes diagnosing complex tooth pain, treating dental trauma, and retreating teeth that need a second chance.
The “don’t ignore this” signs
Tooth pain is not always dramatic. Sometimes it is a slow build. Here are symptoms that often point to a problem inside the tooth:
Common warning signs:
- Lingering sensitivity to cold or heat (lasting more than a few seconds).
- Pain when biting or a feeling that the tooth is “high.”
- Throbbing, spontaneous pain that comes without a trigger.
- Swelling, a gum pimple, or bad taste (possible drainage from an infection).
- A darkened tooth after trauma.
- Pressure in the jaw or face, sometimes mistaken for sinus pain.
If any of these are happening, it is worth getting evaluated sooner rather than later. Tooth infections do not usually “heal on their own.” They often quiet down and then come back louder.
Why saving the natural tooth matters more than people think
Modern dentistry has great replacement options, but your natural tooth is still the gold standard whenever it can be saved.
Keeping your tooth helps you:
- Maintain natural biting and chewing efficiency.
- Avoid shifting of surrounding teeth.
- Protect jawbone health in that area.
- Reduce long-term costs that can come with tooth replacement.
- Keep your smile looking and feeling like you.
Endodontics is often the difference between losing a tooth and keeping it for years, sometimes decades.
When should I see an endodontist instead of a general dentist?
Many general dentists do excellent work, including root canal therapy. But there are times when a case needs a deeper level of focus, magnification, advanced imaging, or specialized techniques.
You should strongly consider seeing an endodontist when:
1) The tooth pain is hard to diagnose:
Some tooth pain is straightforward. Some is not. Pain can radiate, refer to other teeth, or mimic jaw joint or sinus discomfort. Endodontists spend a huge portion of their day diagnosing tooth pain accurately.
2) The root canal anatomy is complex:
Not all teeth have simple root systems. Molars can have multiple canals, curves, tiny branches, and variations that are easy to miss without specialized tools.
3) You have persistent symptoms after treatment:
If you had dental work and the tooth never felt right after, or pain returned months or years later, that is a good reason to see an endodontic specialist.
4) There is dental trauma:
A tooth hit in a fall, sports injury, or accident can suffer internal damage even if it does not crack visibly. Endodontic evaluation can help determine whether the pulp is healing or deteriorating.
5) You want the most conservative option:
When a tooth is borderline, endodontic care can sometimes prevent extraction by treating the infection and preserving the tooth structure.
A practical rule:
If you are dealing with severe pain, swelling, a previously treated tooth that is acting up, or uncertainty about the diagnosis, an endodontist is often the best next step.
Can an endodontist save a tooth that was previously treated with a root canal?
Very often, yes.
A tooth that has had a root canal can still run into trouble later. That does not automatically mean the tooth is “done.” It may simply need retreatment or a more targeted repair.
Here are common reasons a previously treated tooth can flare up again:
Reasons root canal-treated teeth may need help later:
- A canal was missed due to complex anatomy.
- Bacteria re-entered through a cracked filling or leaking crown.
- A new cavity reached deep enough to contaminate the tooth again.
- The tooth developed a crack that was not visible earlier.
- The original infection was severe and took time to fully resolve.
- The root tip area did not heal as expected.
What saving it can look like:
- Root canal retreatment: The previous filling material is removed, canals are cleaned again, disinfected, and resealed.
- Endodontic microsurgery (apicoectomy): If the infection persists around the root tip, a small surgical procedure can remove the inflamed tissue and seal the root end.
- Focused repair and restoration planning: Sometimes the endodontic side is fine, but the tooth needs a better seal on top (a new crown or a replacement restoration).
What matters most is the evaluation.
With proper imaging and testing, it becomes much clearer whether the tooth is a good candidate for retreatment or whether another option makes more sense.
A quick reality check:
If you are told “it needs to come out” without a thorough endodontic assessment, it may be worth getting a second opinion. Not every tooth can be saved, but many can.
What happens if I delay treatment for an infected tooth?
Delaying treatment can turn a manageable problem into a bigger one, sometimes quickly. An infected tooth is not just a “toothache.” It is bacteria and inflammation trapped in a space that is not meant to hold it.
Here is what can happen when you wait:
1) The pain can intensify, then disappear, then return:
This is one of the most misleading patterns. If the nerve tissue inside the tooth dies, pain can temporarily decrease. People assume it “got better.” But the infection can continue spreading silently.
2) The infection can spread beyond the tooth:
A tooth infection can move into the bone around the root tip. That can cause:
- swelling in the gums or face,
- tenderness in the jaw,
- pressure and pain when chewing,
- drainage and bad taste,
- and in some cases, fever or fatigue.
3) You risk an abscess and facial swelling:
Once swelling starts, the situation is no longer just inconvenient. It can become urgent.
4) The tooth can become harder to save:
The longer infection sits, the more tooth structure can weaken from decay, fractures, or repeated breakdown of restorations. Endodontic treatment works best when the tooth can still be properly sealed and restored afterward.
5) You may end up needing more treatment, not less:
Waiting does not usually reduce the total work needed. It often increases it. More infection can mean more appointments, more complexity, and sometimes extraction instead of preservation.
Bottom line: if you suspect an infected tooth, it is not the kind of thing to “watch and see.” It is the kind of thing to diagnose and treat.
What a modern root canal appointment feels like
A lot of people walk in nervous because they are thinking of old stories. Modern endodontic care is different.
In most cases, the goal is that you feel relief, not drama.
Typical steps include:
- Numbing the tooth thoroughly.
- Creating a small opening to access the inside.
- Cleaning and shaping the canals with precision instruments.
- Disinfecting to reduce bacteria.
- Sealing the canals to prevent reinfection.
- Planning the right restoration afterward (often a crown for strength, depending on the tooth).
A key point:
Root canal treatment is not what causes pain. The infection is what causes pain. Endodontic treatment removes the problem.
How to protect your tooth after endodontic treatment
Saving the tooth is step one. Protecting it long-term is step two.
Best habits after treatment:
- Follow the restoration plan. If a crown is recommended, it is usually because the tooth needs reinforcement.
- Avoid chewing hard foods on that side until the tooth is fully restored.
- Keep up with hygiene, especially flossing, since gums help protect the area around the tooth.
- Do not ignore new symptoms like biting pain or swelling. Early fixes are usually simpler.
If you grind your teeth:
A night guard can help prevent cracks and crown damage. Many “mystery root canal failures” are actually bite stress and micro-cracking over time.
A simple way to know when it’s time to come in
If you are wondering whether your tooth issue is “bad enough,” use this checklist:
Come in soon if:
- Pain lingers after hot or cold.
- You wake up with tooth pain or pressure.
- Chewing hurts on one specific tooth.
- You notice swelling, a pimple on the gum, or a bad taste.
- A tooth that had a root canal feels sore again.
- You had trauma and the tooth feels different afterward.
Schedule an appointment with Akemi Dental Specialists
If you are dealing with tooth pain, sensitivity that will not quit, or you suspect an infection, the fastest path to feeling normal again is a proper diagnosis. Endodontic problems tend to get louder when ignored and more manageable when addressed early.
Schedule an appointment with Akemi Dental Specialists to evaluate the tooth, pinpoint the cause, and talk through the most conservative option to relieve pain and protect your smile.